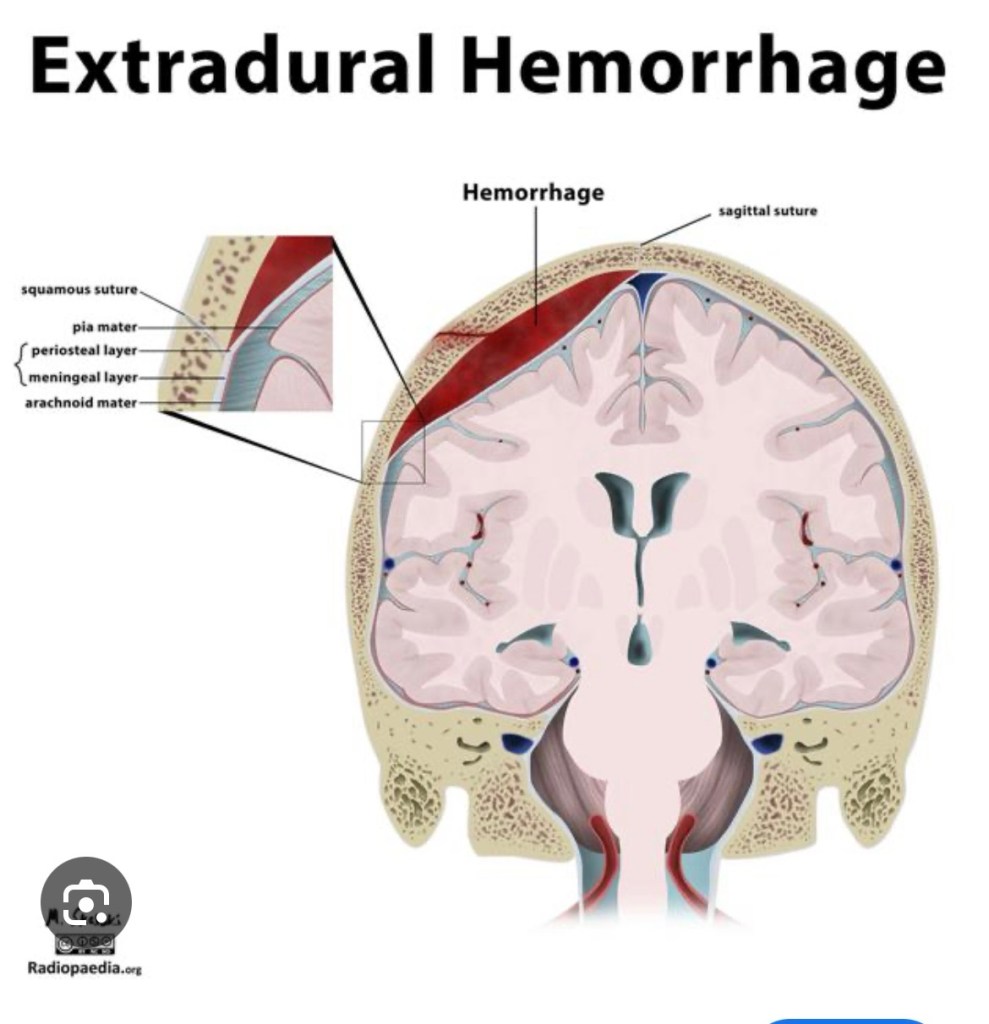
An extradural haematoma is a condition which happens after a head injury. It is a collection of blood that builds up in the space between the skull and the outer covering of the brain, the dura mater.
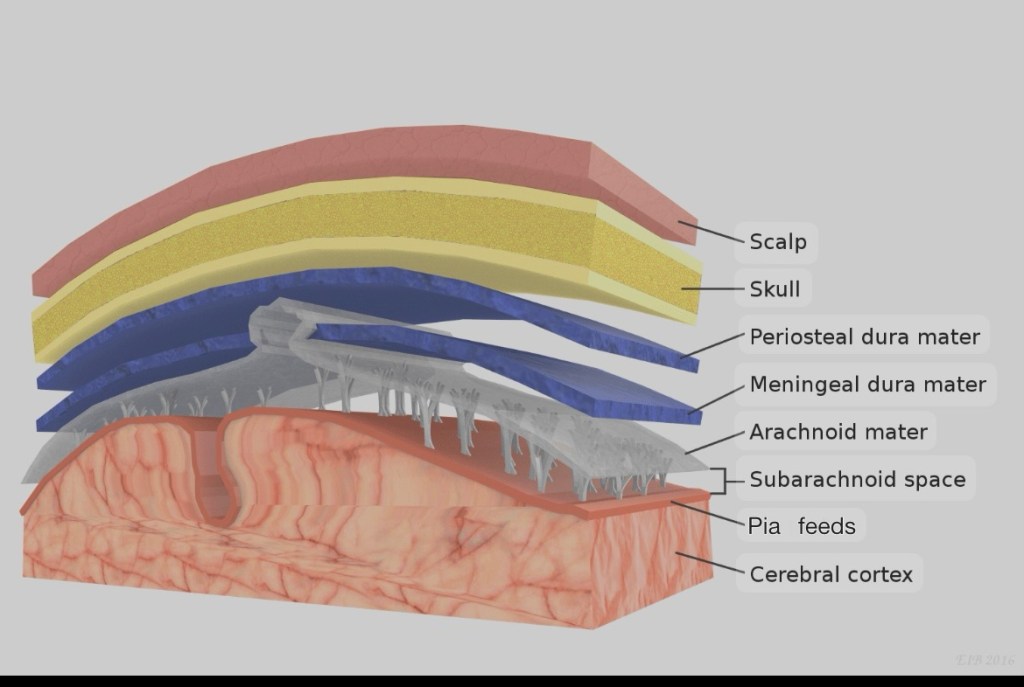
The brain is protected by several layers. First is the scalp, which is the tough skin covering the head. Under that is the skull, a hard bone that protects the brain. Beneath the skull are three layers called the meninges: the dura mater, arachnoid mater, and pia mater.
The brain continues downward as the spinal cord, which passes through an opening at the base of the skull called the foramen magnum and into the spinal canal, which is made up of bones stacked on each other but interlinked called vertebrae. There are a total 33 vertebrae out of 5 are fused as the sacrum and 4 are fused as the coccyx. The stacked arrangement gives the spine flexibility, due the multiple joints. The meninges also cover the spinal cord.
The brain and the spinal cord float in a special fluid called cerebrospinal fluid (CSF), which helps cushion and protect them from injury.
After a head injury, a small fracture in the skull can sometimes tear a blood vessel on the surface of the dura mater—usually an artery called the middle meningeal artery. This causes bleeding in the space between the skull and the dura mater. The resultant expanding clot presses on the brain. The brain has the consistency of ‘Jello’ and can get easily compressed. At first, this pressure may compress the brain to the opposite side of the clot, and then downwards and out through the foramen magnum.
In essence the clot occupies the space previously occupied by the brain, by squeezing it out through the path of least resistance, the foramen magnum.
This wrecks havoc and initially causes headache, nausea and vomiting, followed by confusion and drowsiness progressing into a deepening coma.
There will be weakness of the body on the opposite side of the haematoma, because the right and left hemispheres of the brain control opposite sides of the body.
There will be a dilation of the pupil on the same side of the haematoma because as the brain is pushed to the opposite side, there’s traction on the 3rd cranial nerve as it emerges from the base of the brain and exits via another opening in the skull, the cavernous sinus to supply the eye. As the brain is pushed to the opposite side it gets stretched.
The good thing about extradural haematoma is that there is no injury to the substance of the brain, the symptoms are caused by the compression, hence timely evacuation of the haematoma would result in a complete recovery.
There is what is called the ‘lucid interval’ which occurs in 20%-50% of the cases. This is characterised by a period of lucidity between an initial brief period of loss of consciousness followed by a prolonged period of deepening coma.
Initially following the trauma to the head there’s a loss of consciousness due to ‘concussion’, which is a temporary loss of consciousness, following a head injury, with complete recovery and no neurological deficits.
The patient recovers from the concussion but due to the expanding clot in the extradural space, the patient again loses consciousness and progresses into a deepening coma.
‘Lucid interval’ though not present in all cases of extradural haematoma, if presents is highly indicative of an extra dural haematoma.
I did my surgical residency in Punjab, in the late 80s and 90s, when the secessionist movement was at it’s peak. Trauma a plenty with bombs exploding regularly in front of the police station near the hospital, terrorists opening gunfire in market places and on social gatherings. Once we treated a film crew who were shot at during the shooting of a Punjabi film, ‘Jatt te zameen’. The reigning superstar of the Punjabi film industry Veerendra Singh, who was starring was brought dead to the casualty. He was a cousin of Bollywood film star Dharmendra.
Then there were penetrating head injuries. Among the cases I can recollect there was a young man, who was shot in the head by a 12 bore gun. The cartridges of a 12 bore contain multiple pellets which didn’t penetrate the skull but were embedded all over the scalp. A 14 year old boy shot point blank with the muzzle of the 12 bore kept below his chin. One entire half of his face was blown away. His tongue hanging free and his epiglottis was visible opening and closing with each breath revealing the glottis.
The miraculous thing was both of them survived, the young boy underwent extensive surgery, lost one eye and ear and half of his face but lived to tell the tale.
Another case where a husband attacked his wife with an axe. He opened a good portion of the forehead exposing the frontal lobe of the brain. She too survived to put a case against her husband, for which I had to go to the court as a witness.
Then there were the blunt traumas to the head secondary to road traffic accidents and violence, the victims were invariably under the influence of alcohol and were extremely restless and sometimes violent. One was a boxer who had fallen off the back of a motorcycle, while riding pillion and sustained injury to the back of his head. He was disoriented and restless and almost impossible to restrain. He would easily lift off from the ground two orderlies trying to tie down each arm, like doing a pectoral fly but using two men instead of dumbbells in each hand.
In those days chlorpromazine, an anti psychotic drug was injected to calm down the patient.
Once sedated they could be taken for a Computed Tomography Scan (CT Scan) to assess for brain injuries. The reports could vary from brain contusions, subdural haematomas and of course extradural haematomas.
I was posted as surgery residents in Neurosurgery and as there was no post graduation program in the department of Neurosurgery, I had to fill that role. The pecking order was the Chief, the lecturer and then us. I got exposed to a variety of surgeries.
In neurosurgery like in any surgery the first step is the exposure of the area of interest. In abdominal surgeries the abdomen has to be opened in order to operate, similarly in neurosurgery the skull has to be opened or craniotomy over the required area for the surgical procedure to be performed.
Surgeries had to be performed with the patient in various positions depending on the location of the lesion in the brain. Once we were operating on a portion of the brain called the cerebellum, which is located over the back of the head, just above the neck. The patient had to be seated with his head flexed forwards. Luck followed Murphy’s Law, which decrees, “What can go wrong will go wrong and at the worst possible moment”. In the midst of the surgery, the endotracheal tube or the tube which is inserted via the mouth into the trachea or windpipe, to ventilate the patient and deliver anaesthetic gases got dislodged and came out of the mouth. Because the patient was seated with a flexed neck and covered by surgical drapes, it was not immediately detected, until the brain started swelling and protruding out of the opening in the skull. Immediately the anaesthetist did the impossible of intubating or inserting a endotracheal tube in the seated position. Mind you that’s not an easy task and quoting Shakespeare, “All’s well that ends well”, the patient had an uneventful recovery.
The swelling of the brain was due to the buildup of carbon dioxide and lack of oxygen. Seeing an actual demonstration of this phenomenon made me realise the importance of oxygen in a head injury patient. The brain being already swollen due to trauma gets further swollen due to hypoxia or a lack of oxygen.
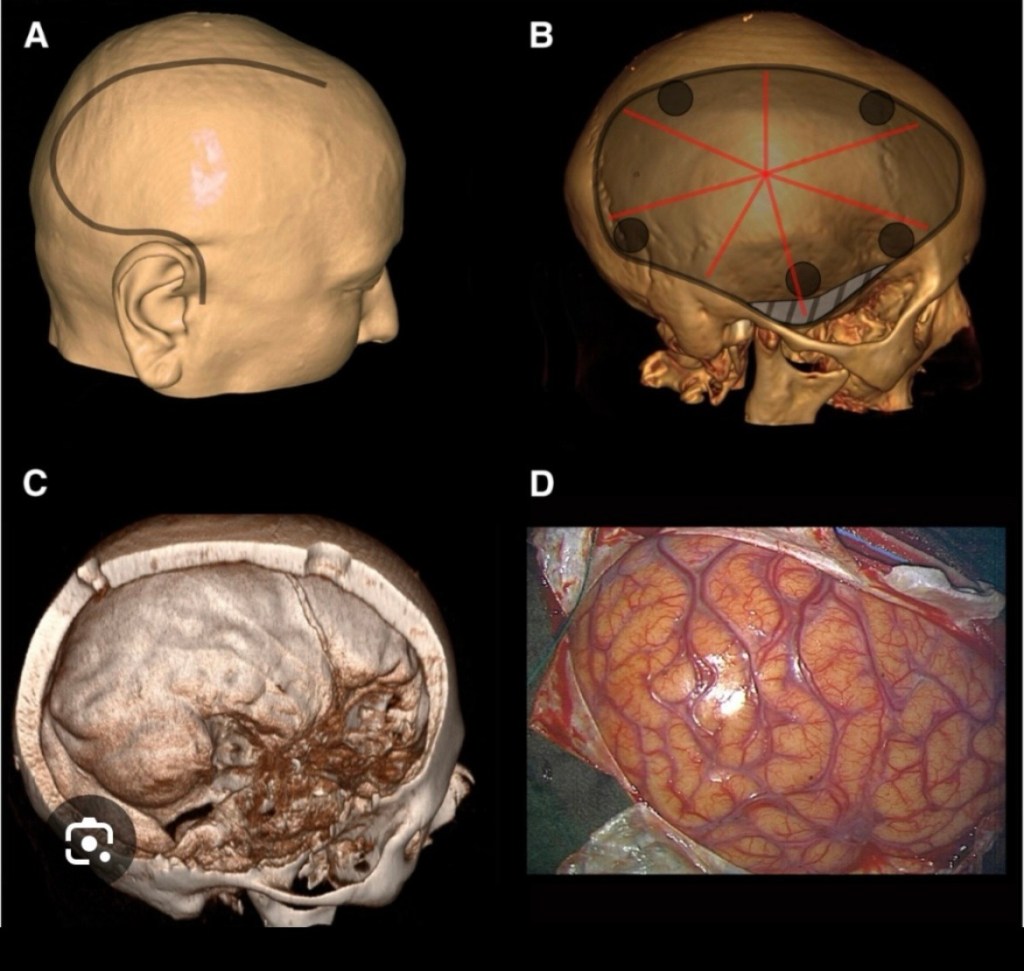
I learnt how to do craniotomies which unlike what is commonly believed about ‘brain surgery’ is fairly easy. First is to plan craniotomy according to the location of the lesion, then if possible to avoid crossing the midline as there’s the saggital sinus in the midline. The saggital sinus is a channel carrying venous blood enclosed by the dura mater. Also avoid going too posteriorly as the transverse sinus crosses there.
The logic being if you drill into the sinus you will encounter torrential bleeding which will be very difficult to control.
After planning the location of your craniotomy an incision has to be made on the scalp. This is in the form of a flap with a wide pedicle to prevent devascularisation or loss of blood supply to the scalp the flap preferably should be within the hairline as to be cosmetic.
A very popular question which is asked to residents in neurosurgery is ” What is the most important covering of the brain?” The answer is the scalp and not the skull as most people believe!
I encountered so many craniotomies done in other hospitals where there’s a defect in the skull covered by only scalp. Rather than cutting a flap of bone, a hole was nibbled in the skull and the scalp was sutured back over the defect. The patient is otherwise perfectly alright except for having a concavity on the head.
We treated this by sending the patient to the dental department where they take an impression of the defect and make a prosthesis, made out of the same material dentures are made of, to fit the defect.
The scalp again had to be opened and the prosthesis always fitted perfectly, sometimes it required some minor adjustments. The prosthesis was then anchored over the defect and the scalp closed. The patient had satisfactory contour of his head.
These days thanks to 3D printing a perfect prosthesis can be made to fit in the defect, like a hand in a glove.
Our plastic surgeon once used the flat bone from the ileum, which is the large bone deep to the buttocks. He only took just the outer layer of the bone along with it’s supplying blood vessel and placed it to cover a defect in the skull. The bone had a natural convexity matching that of the skull and the blood vessel was anastomosed or joined to the blood vessel in neighbourhood and voila! The patient had a living bone covering the defect.
Returning to the subject of crainotomies, once the location is planned and an incision is made in the scalp, holes called ‘burr holes’ are drilled on the skull in a polygonal pattern, either pentagonal, hexagonal, octagonal or nonagonal pattern depending on the size of the opening required. While drilling the holes the dura mater is not punctured.
C. Surface of dura exposed D. Surface of brain exposed
Then a Gigli saw wire is passed between adjacent holes and the intervening bone is cut. When all adjacent holes are connected a bony flap is raised having a polygonal shape. The advantage of having this bone flap was it could be replaced over the defect once the surgery was completed, avoiding the concave defect in the skull.
The Gigli saw is a very simple but versatile instrument. It consists of a thin, twisted stainless steel wire with serrated edges. Like a piano wire. It has detachable handles at each end for gripping. Designed to cut through bone with a back-and-forth sawing motion. It can easily threaded through two adjacent holes and the intervening bone cut.


Ironically it was originally designed by a Obstetrician and was used to divide the symphysis pubis in cases of obstructed labour, when Cesarean section was not safe.
Once the skull is opened, depending on the pathology, either on the dura mater or on or within the brain, an opening can be made in the dura mater to expose the surface of the brain.
I was gradually initiated, first I was allowed to make an incision on the scalp. The scalp being very vascular, the bleeding had to be controlled by holding the inner layer and everting the scalp.
Next I was allowed to make the burr holes, this was done using what is called the’Hudson brace’ which essentially is like a carpenter’s drill. It had two tips, one is called the perforator which we use to penetrate the skull and the other is called the burr, which is used to widen the hole.
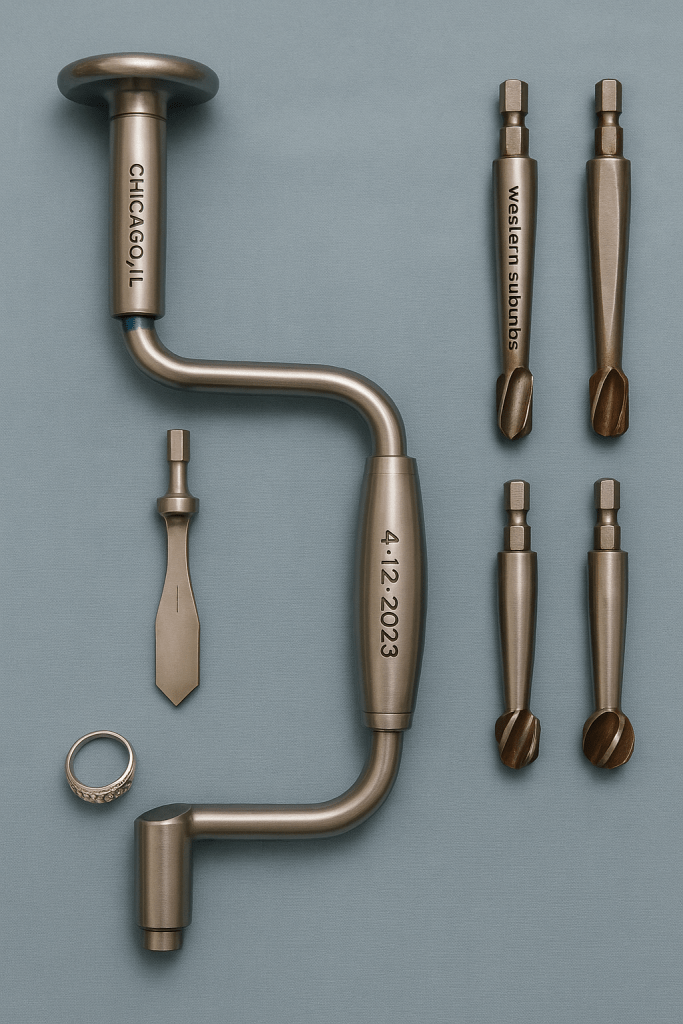
Initially the perforator is used till the thickness of the skull is penetrated and a small opening is seen at the base of hole. Next it is widened with the burr. It blunt tip but has bevels around it’s circumference and widens the hole.
Once burr holes made in a polygonal pattern over the skull we next got to join them with a Gigli saw. The wire of the Gigli saw is threaded through one burr hole and brought through an adjacent burr hole. Then the handles are attached and the wire is moved in a to and fro motion. The wire cuts the bone smoothly and once all the holes are connected, we have a bone flap which can be lifted off.
The skull because of it’s dome shaped design is very tough and does not fracture easily but the portion of the between the ear and forehead, behind the eye and above the zygoma or cheek bone is the weakest portion. This portion is called temporal region also colloquially known as the temple.
This area includes parts of several bones—primarily the temporal bone—and it’s a sensitive region because it has relatively thin bone and several important blood vessels and nerves running through it. That’s why a blow to the temple can be particularly dangerous.
In most martial arts the blows are aimed at this region as this can result in a KO or knockout. In Karate, Kung Fu and Muay Thai there is the round house kick which aims at hitting the temporal region with the side of foot or shin.
The protective gear worn is designed to protect the temporal region. Trauma to this region can result in fracture or in children who have an elastic bone just bending without breaking. On the surface of the underlying dura mater lyes the middle meningeal artery, the anterior branch of this artery is prone to injury and bleeding and an expanding haematoma collects in this region.
Before the advent of CT Scan diagnosis of an extradural haematoma was not very easy. A plain x-ray of the skull could show the calcified pineal body being pushed to one side. A cerebral angiography could be done which is injecting a dye which is radio-opaque into the internal carotid artery. An x-ray taken would outline the brain and demonstrate compression and deviation.
When there’s adequate suspicion an exploratory burr hole can be made on the side of the trauma. This is normally made just above the zygoma or cheek bone, midway between the eye and ear. You will encounter blood clots which will confirm your diagnosis. Then the same burr hole can be enlarged using a bone nibbler and the clot evacuated or burr holes made around it which are joined and a bone flap is raised. The advantage of creating a flap is there’s no defect and concavity in the skull.
With the advent of CT Scan things have become easy, a convex opacity is seen in the scan and the degree of compression and deviation of the brain from the midline can be assessed.

When my lecturer became confident in my abilities to do a craniotomy he allowed me to do a craniotomy for a case of extra dural haematoma. After reviewing the CT Scan he instructed me to make a ‘trauma flap’ on the scalp and then do the craniotomy. He drew the trauma flap for me, which started from the forehead on one side without crossing the midline and ran parallel to the midline posteriorly, then took a curve downwards and returns to end just above the ear.
I’m happy to say that the surgery was successful and the patient’s recovery was uneventful.
After completing my surgical residency I joined a hospital in a remote rural area, the population was 70% tribal. I had a lot of training but now was to put it into practice.
One night a young patient was brought unconscious to the casualty. He was a travelling salesman who sold blankets. He had gone to a nearby village to sell his blankets and had some altercation with the villagers who were drunk with the local brew ‘mahua’. One villager hit him on his right temple with a lathi. He lost consciousness momentarily but recovered and then went with his companions to register a complaint in the local police station. After registering a complaint he returned to the dharamshala where he was staying and lost consciousness.
His companions took him to the district hospital but they were unable to do anything for him. He was then brought to our hospital in the night, where the emergency doctors saw him and admitted him.
I saw him in the morning, he was deeply comatosed and both his pupils were dilated.
Going by the history of lucid interval I could come to a diagnosis of extra dural haematoma but since we were in a remote area we didn’t have the facilities for a CT Scan to confirm my diagnosis.
I was faced with a conundrum, if I referred this patient to the major cities which were 200 kms away, by the time he reached he would be unsalvageable. We had the equipment to perform a craniotomy so I explained the situation to the relatives and after taking they’re consent I proceeded on.
The anaesthetist said that he was so deeply comatosed that he would intubate him but not give any anaesthetic gases, only oxygen.
I positioned him to left side with right side of the head up. I first made a vertical incision over the temporal region and made a burr hole, I got got clots from the burr hole, confirming my diagnosis.
Next I thought whether to enlarge the burr hole or raise a bone flap. I opted for the bone flap. I made a trauma flap on the scalp and five burr holes around the first one. I joined the holes using a Gigli’s saw. Once I lifted the bone flap I could see the dark red clot. After evacuating the clot I could see the bleeding vessel which I ligated. Then I took stitches hitching the dura to the craniotomy opening. Then a drain was placed on the dura and the bone flap was replaced and the scalp closed.
By the time I finished the surgery the patient regained consciousness and began to move. The anaesthetist had to now supplement him with anaesthetic gases.
The patient made a dramatic recovery and only had hemipareisis or weakening of the left side of the body. This would also would improve with time.
I consider this one of the most satisfying moments of my career when I could use my knowledge and expertise to save a life. This was the reason why I became a surgeon.